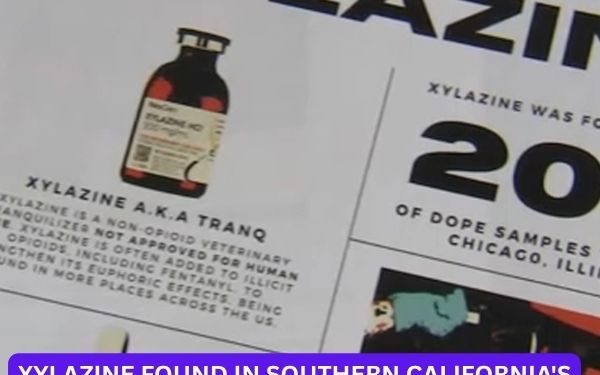
LOS ANGELES — A new and deeply troubling threat is intensifying California’s overdose crisis. Xylazine, a powerful veterinary sedative known on the streets as “tranq” or the “zombie drug,” is now appearing across multiple Southern California counties, triggering widespread concern among health experts, law enforcement, and outreach workers.
Originally designed to sedate large animals, xylazine is now being laced into fentanyl, making an already deadly opioid even more dangerous. The mixture causes prolonged blackouts, deep sedation, and horrific skin ulcers—wounds that sometimes rot tissue down to the bone. Most critically, xylazine doesn’t respond to Narcan (naloxone), the standard overdose reversal medication.
“We’re Entering a New Phase of the Crisis”
Dr. Joseph Friedman, an addiction researcher at UC San Diego, said the rapid spread of xylazine represents a grim “new normal” in the opioid epidemic. His research confirms its growing presence in fentanyl samples across Southern California and even in nearby Mexican border cities.
“This is not the same drug crisis we were fighting five years ago,” Friedman said. “We’re entering uncharted territory.”
In Los Angeles’ Skid Row, home to one of the country’s largest unhoused populations, the crisis is already visible. Health workers report seeing an alarming rise in flesh wounds, abscesses, and zombie-like symptoms among people who unknowingly used fentanyl contaminated with tranq.
Drug Cartels Branding Tranq-Laced Fentanyl
Federal authorities say traffickers are using colored dyes—like purple—to brand fentanyl batches laced with xylazine, making the drug visually distinct on the street. In one seizure in downtown L.A., DEA agents recovered enough fentanyl-xylazine powder to “kill everyone in downtown Los Angeles.”
“What makes this even more dangerous is that xylazine is not a controlled substance,” said one DEA official. “That means many labs don’t test for it, so it often slips through undetected.”
So far this year, U.S. Customs and Border Protection has seized over 48,000 pounds of narcotics, and xylazine is showing up with increasing frequency.
No Antidote. No Easy Fix.
What makes tranq especially terrifying is that there’s no approved antidote. Narcan can reverse fentanyl overdoses, but it doesn’t work on xylazine, which isn’t an opioid. The result: longer-lasting blackouts and higher fatality rates—especially among vulnerable populations.
On the frontlines, harm reduction workers are calling for immediate solutions: broader drug testing, better surveillance, expanded health services, and real-time public alerts.
“This isn’t just about drug users,” said a public health nurse in L.A. “This is about a shifting crisis that could affect anyone.”
For those living with addiction, however, the rise of tranq adds another layer of danger to an already deadly reality.
“We know what’s in it,” one Skid Row resident said. “We just don’t have anything else. It’s a gamble we take every day.”